Study Finds PCC a Safe Alternative to Plasma in Heart Surgery
PCC improved prothrombin time and INR versus plasma
06/30/2022
Peggy Peck, Editor-in-Chief, BreakingMED™
Kevin Rodowicz, DO, Assistant Professor, St. Luke’s University/Temple University
In a single-center, prospective, randomized trial of 100 complex cardiac surgery patients, there was no difference in post-operative bleeding between patients receiving PCC or plasma.
Fewer patients in the PCC group required intraoperative red blood cell transfusion after treatment, and adverse outcomes were similar between groups.
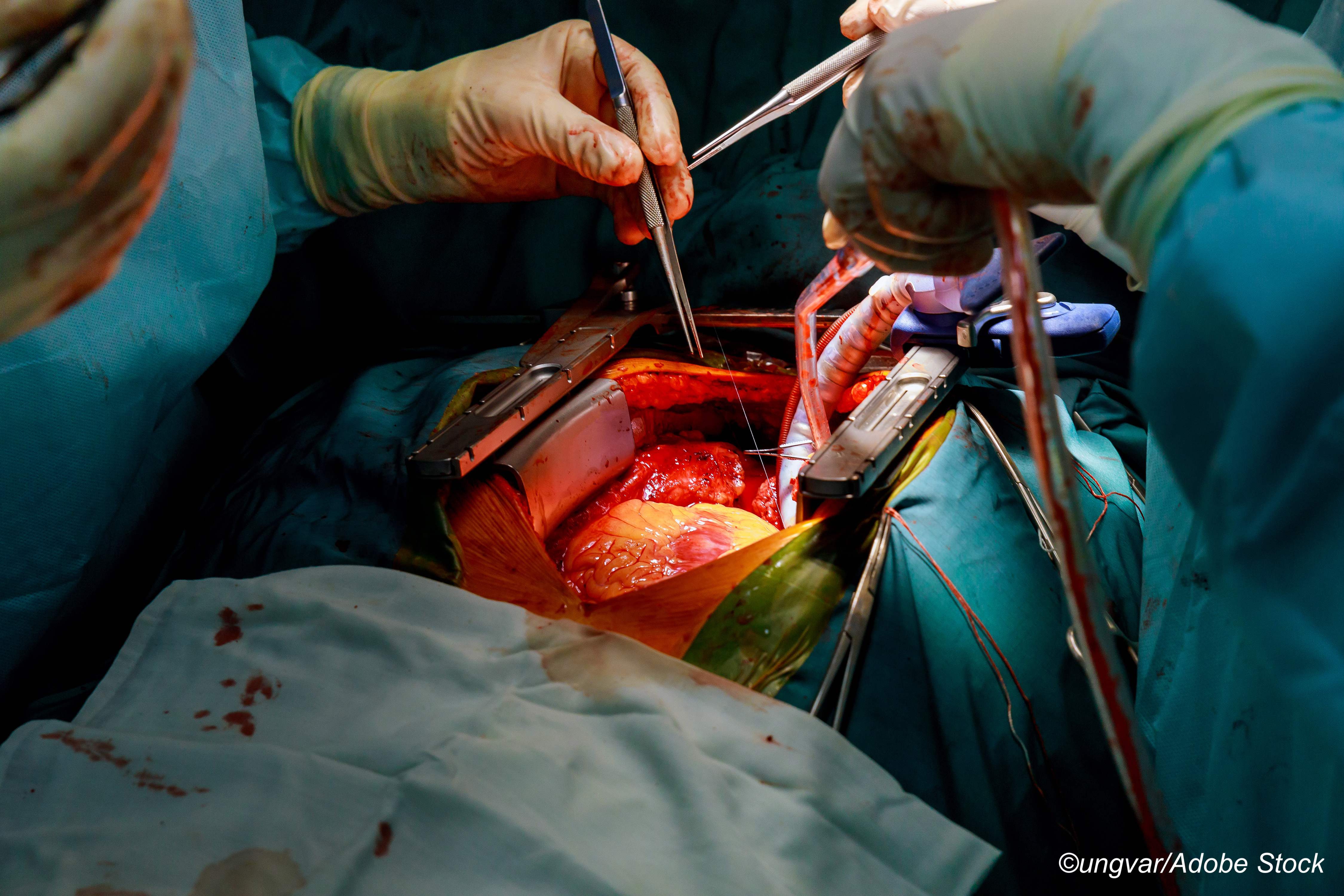
A single-center, prospective, randomize trial by Mayo Clinic researchers confirmed the benefit of using prothrombin complex concentrate (PCC) rather than plasma to treat patients who develop excessive microvascular bleeding following heart surgery, such as aortic valve replacement, complicated coronary artery bypass grafts (CABG), or repeated sternotomy, according to findings published online by JAMA Surgery.
Mark M. Smith, MD, of the Division of Cardiovascular and Thoracic Anesthesia, Department of Anesthesiology and Perioperative Medicine, Mayo Clinic College of Medicine and Science in Rochester, Minnesota, and colleagues wrote that patients randomized to PCC had significant improvement in the secondary outcome measures of prothrombin time (PT) and coagulation international normalized ratio (INR).
"After treatment, patients in the PCC arm had a greater improvement in PT (effect estimate, −1.37 seconds [95% CI, −1.91 to −0.84]; P<0.001) and INR (effect estimate, −0.12 [95% CI, −0.16 to −0.07]; P<0.001)," they wrote. But for the primary endpoint—post-operative bleeding, as measured by chest tube output in the immediate post-operative hours—there was no significant difference.
 Additionally, only seven of 51 patients randomized to PCC had intraoperative red blood cell (RBC) transfusion versus 15 of the 49 patients who received plasma, 13.7% versus 30.6% (P=0.04), which Smith et al termed an important outcome because it "relates to the potential reduction or avoidance of allogeneic transfusions, including allogeneic plasma avoidance by way of PCC substitution and reduced hemodilution necessitating RBC transfusion seen with large-volume plasma transfusion… This is particularly relevant at a time when shortages in allogeneic blood products are a reality and blood banks are commonly under supplied."
Additionally, only seven of 51 patients randomized to PCC had intraoperative red blood cell (RBC) transfusion versus 15 of the 49 patients who received plasma, 13.7% versus 30.6% (P=0.04), which Smith et al termed an important outcome because it "relates to the potential reduction or avoidance of allogeneic transfusions, including allogeneic plasma avoidance by way of PCC substitution and reduced hemodilution necessitating RBC transfusion seen with large-volume plasma transfusion… This is particularly relevant at a time when shortages in allogeneic blood products are a reality and blood banks are commonly under supplied."
After screening 756 patients, the researchers eventually randomized 100; mean age was 66.8 years, and most were men (61%). The study was conducted at the Mayo campus in Olmsted County, an area with an extremely homogeneous population, so not surprisingly, 98% of the participants were White, 1% Black, and 1% Hispanic.
There were more men in the plasma group (35 of 49) and more patients with a history of atrial fibrillation in the PCC group (6 versus no AFib patients in the plasma group).
"Patients in the plasma group had a higher baseline hemoglobin level compared with the PCC group (mean [SD], 12.47 [1.55] g/dL versus 11.65 g/dL [1.58]; P=0.01)… In assessment of the pre-to-post-treatment impact of the interventions on laboratory values, patients in the PCC arm had a higher posttreatment hemoglobin level (mean [SD], 9.81 [1.68] versus 10.51 [1.62]; estimated treatment effect, 0.81 g/dL [95% CI, 0.20-1.43]; P=0.01), which may be explained by higher cell saver volume in the PCC group (median [IQR], 633 (484-1018) mL versus 702 [472-917] mL; and greater improvements in PT (effect estimate, −1.37 seconds [95% CI, −1.91 to −0.84]; P<0.001) and INR (effect estimate, −0.12 [95% CI, −0.16 to −0.07]; P<0.001) compared with the plasma group," they wrote.
Chest tube output was measured from the initial post-op period through midnight of the next day, and the median chest tube output in the plasm group was 1,022 mL versus 937 mL (P=0.84).
In the post-operative period, there were fewer RBC transfusions in the PCC group than in the plasma group—15 patients versus 22 patients—but the difference was not significant.
"To our knowledge, this is the first prospective randomized clinical trial comparing PCC use with plasma use therapies in patients undergoing cardiac surgery," Smith et al wrote. "The main findings of this study were that perioperative bleeding and transfusion requirements were similar between those receiving plasma and PCC, except for significantly lower posttreatment intraoperative RBC transfusions for patients receiving PCCs. Patients receiving PCCs also had a greater improvement in PT/INR values compared with those receiving plasma. Perioperative allogeneic transfusion avoidance was higher in patients receiving PCCs. There were no differences in adverse outcomes between groups."
Study limitations included an extended enrollment period (August 2016 through January 2022) due to "uncontrollable variables (e.g., Covid-19 pandemic-related research restrictions and surgical volume fluctuations, study-staff absences, and competing studies)." Additionally, the results may not be generalizable due to the trial’s single-center design and lack of diversity in the population studied.
Smith and colleagues concluded that the results they reported "suggest an overall similar efficacy and safety profile, with a lower rate of posttreatment intraoperative RBC transfusion, improved PT/INR correction, and higher incidence of allogeneic transfusion avoidance in patients receiving PCCs compared with plasma in this clinical context."
Disclosures
Smith reported recieving grants from CSL Behring for investigator-initiated research during the conduct of the study.
Sources
Smith, MM et al "Prothrombin complex concentrate vs plasma for post–cardiopulmonary bypass coagulopathy and bleeding: A randomized clinical trial" JAMA Surg 2022; DOI: 10.1001/jamasurg.2022.2235.