Do GLP-1 RAs Increase Risk of Gallbladder, Biliary Diseases?
Systematic review/meta-analysis suggests greater risk with higher doses,longer Tx
03/29/2022
John McKenna, Associate Editor, BreakingMED™
Kevin Rodowicz, DO, Assistant Professor, St. Luke’s University/Temple University
Treatment with glucagon-like peptide-1 receptor agonists (GLP-1 RAs) was linked to increased risks for gallbladder and biliary diseases, particularly cholelithiasis, cholecystitis, and biliary disease, according to findings from a systematic review and meta-analysis.
Among all included trials, GLP-1 RA use was associated with higher risks of gallbladder or biliary diseases at higher doses compared with lower doses and with longer duration of use compared with shorter duration.
Treatment with glucagon-like peptide-1 receptor agonists (GLP-1 RAs) was linked to increased risks for a slew of gallbladder and biliary diseases, according to findings from a systematic review and meta-analysis.
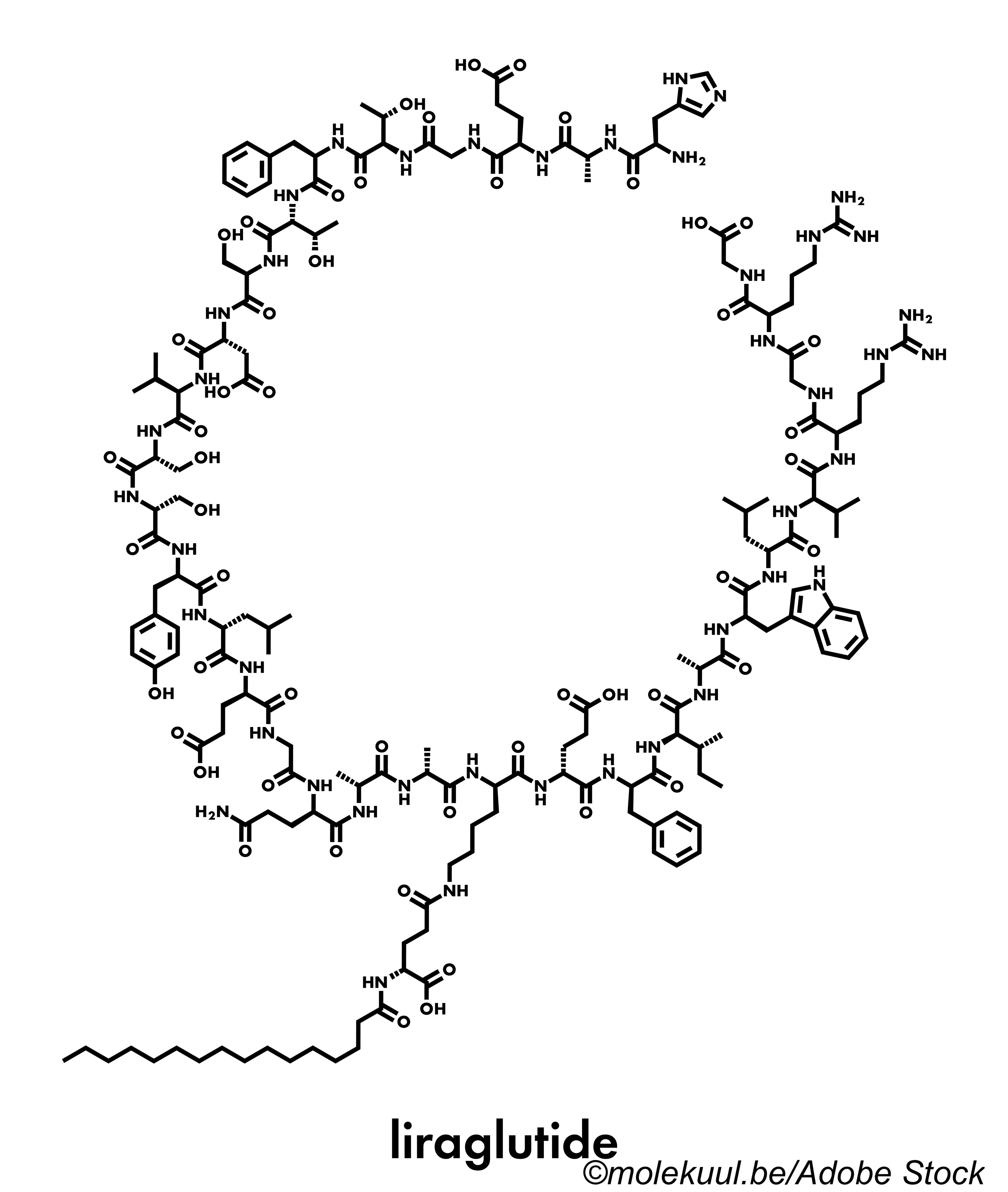
GLP-1 RAs, such as liraglutide, semaglutide, dulaglutide, and others, are currently recommended for patients with type 2 diabetes (T2D) and at higher doses for obesity; however, several randomized trials have shown higher rates of gallbladder- and biliary-related conditions in these patients—a particular concern given the widespread use of these drugs, Huabing Zhang, MD, of Chinese Academy of Medical Sciences and Peking Union Medical College in Beijing, China, and colleagues explained in JAMA Internal Medicine.
To determine whether these adverse events are a class effect of GLP-1 RAs, and to evaluate the differential risk for these conditions based on whether they’re being used for T2D or obesity, Zhang and colleagues conducted a review of 76 randomized trials involving data from over 100,000 patients.
"This systematic review and meta-analysis of 76 randomized clinical trials found that randomization to treatment with GLP-1 RAs compared with placebo or active controls was associated with increased risk of the composite outcome of gallbladder or biliary diseases and for cholelithiasis, cholecystitis, and biliary diseases," Zhang and colleagues found. "Risk was increased in trials of patients treated for diabetes and for weight loss and was higher in the trials for weight reduction. Higher doses and longer duration of GLP-1 RAs treatment were also associated with increased risk of gallbladder or biliary diseases, although the association was not statistically significant."
The study authors concluded that physicians "should be concerned about the increased risk of gallbladder or biliary disease associated with GLP-1 RA use, especially at the higher doses recommended for weight loss. In addition, future trials should prespecify gallbladder and biliary diseases as potential adverse events, and fully test for and report on these outcomes."
For this review and meta-analysis, Zhang and colleagues searched MEDLINE, Cochrane Library, EMBASE, and Web Science from database inception through June 30, 2021, for randomized trials of GLP-1 RA medications—albiglutide, dulaglutide, exenatide, liraglutide, lixisenatide, or semaglutide—that also reported adverse events of gallbladder or biliary diseases. Pooled relative risks (RRs) were calculated via random or fixed-effects models, and quality of evidence was assessed using the GRADE framework.
"The primary outcome was a composite of gallbladder or biliary diseases, including gallbladder disorders and biliary-related events," the review authors explained. "Secondary outcomes were three subcategories of gallbladder and biliary diseases, including bile duct obstruction, stenosis, and stone; biliary colic, cyst, and fistula; biliary tract cancer; cholecystectomy, cholecystitis, and cholelithiasis; and cholangitis."
The meta-analysis included a total of 76 trials involving 103,371 patients; mean patient age was 57.8 years, and 40.5% were women. The majority of trials were at low or some risk for bias, and the quality of evidence was generally rated as high.
"Among all included trials, randomization to GLP-1 RA treatment was associated with increased risks of gallbladder or biliary diseases (RR, 1.37; 95% CI, 1.23-1.52); specifically, cholelithiasis (RR, 1.27; 95% CI, 1.10-1.47), cholecystitis (RR, 1.36; 95% CI, 1.14-1.62), and biliary disease (RR, 1.55; 95% CI, 1.08-2.22)," Zhang and colleagues found. "Use of GLP-1 RAs was also associated with increased risk of gallbladder or biliary diseases in trials for weight loss (n=13; RR, 2.29; 95% CI, 1.64-3.18) and for type 2 diabetes or other diseases (n=63; RR, 1.27; 95% CI, 1.14-1.43; P<0.001 for interaction). Among all included trials, GLP-1 RA use was associated with higher risks of gallbladder or biliary diseases at higher doses (RR, 1.56; 95% CI, 1.36-1.78) compared with lower doses (RR, 0.99; 95% CI, 0.73-1.33; P=0.006 for interaction) and with longer duration of use (RR, 1.40; 95% CI, 1.26-1.56) compared with shorter duration (RR, 0.79; 95% CI, 0.48-1.31; P=0.03 for interaction)."
As for specific drugs, treatment with either liraglutide or dulaglutide were associated with increased risk of gallbladder or biliary diseases (RR 1.79 and 1.35, respectively); subcutaneous semaglutide and exenatide were associated with increased risk (RR 1.28 and 1.23, respectively), but this increase was not statistically significant; and oral semaglutide, lixisenatide, and albiglutide did not increase risk.
In an editorial accompanying the review, Shanzay Haider, MD, and Kasia J. Lipska, MD, MHS, both of Yale School of Medicine in New Haven, Connecticut, noted that the analysis by Zhang and colleagues "leaves some open questions. It is unclear whether the gallbladder and biliary complications were directly attributable to the weight loss associated with GLP-1 RA use or with other mechanisms. The higher-risk signal in GLP-1 RA trials for weight loss indications may be attributable to more weight loss achieved in those trials and/or to the higher doses of GLP-1 RAs typically used for weight loss. Which patients are at the greatest risk for developing gallbladder and biliary complications is also unclear. Without patient-level data, the authors could not conduct analyses to examine the differences by age, sex, or other clinical factors."
Haider and Lipska argued that the findings by Zhang et al need to be considered in the context of a given patient’s situation. They cited an example in which a 64-year-old patient with T2D and a history of myocardial infarction was interested in initiating treatment with GLP-1 RAs.
"The patient described in this commentary was interested in losing weight, and GLP-1 RA use is typically associated with modest weight loss," they explained. "Because he had established cardiovascular disease, his risk of nonfatal myocardial infarction, nonfatal stroke, and mortality can be estimated to be 108, 120, and 108 events, respectively, per 1000 persons in the next 5 years; GLP-1 RA treatment is associated with absolute reductions of 8, 16, and 13 events, respectively, per 1,000 persons during the same period. These reductions are modest, and individual patients may place different values on avoiding these outcomes."
Meanwhile, based on this meta-analysis, they noted GLP1- RAs would be associated with an excess of "approximately 1.3 gallbladder or biliary events per 1,000 persons treated per year." What’s more, other factors, including treatment costs, insurance coverage, and preference for injectables also need to be taken into account. The patient in the example eventually chose to start weekly GLP-1 RA therapy with the caveat that they were interested in whether there was a way to mitigate gastrointestinal adverse events associated with the drugs.
"Ultimately, the decision to start, continue, or change the dose of a GLP-1 RA should be reached through a collaborative and individualized discussion between a clinician and a patient," Haider and Lipska concluded.
Review/meta-analysis limitations cited by the authors included the potential that information on biliary-related events may not have been fully reported; the included trials were not specifically designed to evaluate gallbladder and biliary disease risks with these treatments; the authors couldn’t use patient-level data to evaluate outcomes; and the small number of events in subgroups may have led to underpowered subgroup analyses.
Disclosures
The review authors had no relevant relationships to disclose.
Lipska reported grants from the US National Institutes of Health and other support from the Centers for Medicare & Medicaid Services and UpToDate.
Sources
Zhang H, et al "Association of glucagon-like peptide-1 receptor agonist use with risk of gallbladder and biliary diseases: A systematic review and meta-analysis of randomized clinical trials" JAMA Intern Med 2022; DOI: 10.1001/jamainternmed.2022.0338.
Haider S, Lipska KJ "Glucagon-like peptide-1 receptor agonists—How safe are they?" JAMA Intern Med 2022; DOI: 10.1001/jamainternmed.2022.0335.